The City of Bangor follows the guidance from the US CDC and Maine CDC regarding COVID 19
Click on the + and – signs next to each title below to read the content in each section.
Key Things to Know About COVID-19 Vaccines
Click here to find a vaccination site near you
COVID-19 vaccines are effective at protecting you from COVID-19, especially severe illness and death. COVID-19 vaccines reduce the risk of people spreading the virus that causes COVID-19. If you are fully vaccinated, you can resume activities that you did before the pandemic.
COVID-19 vaccines teach our immune systems how to recognize and fight the virus that causes COVID-19. It typically takes 2 weeks after vaccination for the body to build protection (immunity) against the virus that causes COVID-19. That means it is possible a person could still get COVID-19 before or just after vaccination and then get sick because the vaccine did not have enough time to build protection. People are considered fully vaccinated 2 weeks after their second dose of the Pfizer-BioNTech or Moderna COVID-19 vaccines, or 2 weeks after the single-dose Johnson & Johnson’s Janssen COVID-19 vaccine.
- FDA-authorized COVID-19 vaccines help protect against Delta and other known variants.
- These vaccines are effective at keeping people from getting COVID-19, getting very sick, and dying.
- To maximize protection from the Delta variant and prevent possibly spreading it to others, you should wear a mask indoors in public if you are in an area of substantial or high transmission even if you are fully vaccinated.
- We don’t know how effective the vaccines will be against new variants that may arise.
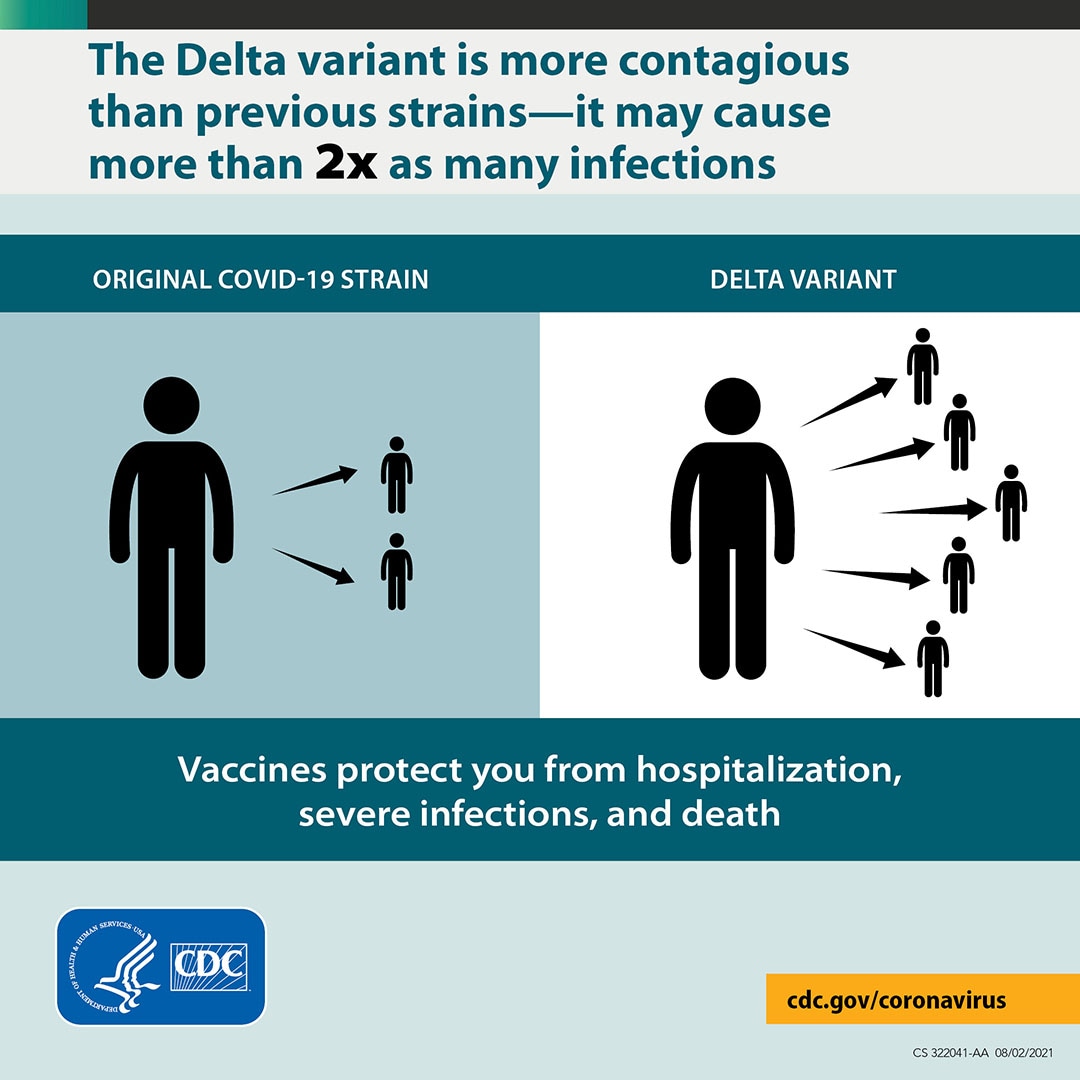
The Delta variant causes more infections and spreads faster than earlier forms of the virus that causes COVID-19. It might cause more severe illness than previous strains in unvaccinated people.
- Vaccines continue to reduce a person’s risk of contracting the virus that cause COVID-19, including this variant.
- Vaccines continue to be highly effective at preventing hospitalization and death, including against this variant.
- Fully vaccinated people with breakthrough infections from this variant appear to be infectious for a shorter period.
- Get vaccinated and wear masks indoors in public spaces to reduce the spread of this variant.
Click here for more information about the different vaccines
What We Know About the Delta Variant
The Delta variant causes more infections and spreads faster than early forms of SARS-CoV-2
- The Delta variant is more contagious: The Delta variant is highly contagious, more than 2x as contagious as previous variants.
- Some data suggest the Delta variant might cause more severe illness than previous strains in unvaccinated persons. In two different studies from Canada and Scotland, patients infected with the Delta variant were more likely to be hospitalized than patients infected with Alpha or the original virus strains.
- Unvaccinated people remain the greatest concern: Although breakthrough infections happen much less often than infections in unvaccinated people, individuals infected with the Delta variant, including fully vaccinated people with symptomatic breakthrough infections, can transmit it to others. CDC is continuing to assess data on whether fully vaccinated people with asymptomatic breakthrough infections can transmit. However, the greatest risk of transmission is among unvaccinated people who are much more likely to contract, and therefore transmit the virus.
- Fully vaccinated people with Delta variant breakthrough infections can spread the virus to others. However, vaccinated people appear to be infectious for a shorter period: Previous variants typically produced less virus in the body of infected fully vaccinated people (breakthrough infections) than in unvaccinated people. In contrast, the Delta variant seems to produce the same high amount of virus in both unvaccinated and fully vaccinated people. However, like other variants, the amount of virus produced by Delta breakthrough infections in fully vaccinated people also goes down faster than infections in unvaccinated people. This means fully vaccinated people are likely infectious for less time than unvaccinated people.
Using Cloth Face Coverings
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html
Download the Use and Care of Cloth Masks instruction sheet.
Staying home and social distancing are still the best ways to protect yourself and others. However, US CDC now recommends the additional, voluntary step of wearing a cloth face covering when you must visit public places, such as the grocery store or pharmacy.
Wearing a mask helps protect others. You can have, or pass on COVID-19 without having any symptoms. That’s why wearing a mask, even if you don’t feel sick can be a good idea. If you have a job in a public setting, wearing a mask while at work may provide an even bigger benefit to the community, because of the number of people you encounter in a day.
How to Wear a Mask

Masks should -
• fit snugly but comfortably against the side of your face
• be secured with ties or ear loops
• include multiple layers of fabric
• allow you to breathe without restriction
• be able to be machine-washed and dried without damage or
change to shape
People should continue to practice social distancing, keeping 6 feet apart and
washing hands/using hand sanitizer frequently.
Removing a Mask
When removing a mask or face covering, be careful not to touch your eyes,
nose, or mouth. Wash hands immediately after removing.
Cleaning Masks
Cloth face coverings should be machine-washed and dried at home after each use with usual laundering practices. If you have a mesh bag, laundering inside the bag is recommended.
Additional CDC Info on Cloth Face Coverings
Coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated or otherwise unable to remove their own mask.
View instructions on how to make cloth masks. If you plan to sew masks, we recommend the use of cloth ties, as elastic or rubber can break down with frequent laundering.
Symptoms, Self-Checker, and Testing Information
The following symptoms may appear 2-14 days after exposure:
- Fever
- Cough
- Shortness of breath
Call your doctor: If you think you have been exposed to COVID-19 and develop a fever and symptoms, such as cough or difficulty breathing, call your healthcare provider for medical advice.
US CDC has added a Self Checker to their symptoms web page to help you make decisions and seek appropriate medical care.
Older adults and people who have severe underlying medical conditions like heart or lung disease or diabetes seem to be at higher risk for developing more serious complications from COVID-19 illness.
Who should get tested for current infection
- People who have symptoms of COVID-19.
- Most people who have had close contact (within 6 feet for a total of 15 minutes or more over a 24-hour period) with someone with confirmed COVID-19.
- Fully vaccinated people should be tested 3-5 days following a known exposure to someone with suspected or confirmed COVID-19 and wear a mask in public indoor settings for 14 days or until they receive a negative test result.
- People who have tested positive for COVID-19 within the past 3 months and recovered do not need to get tested following an exposure as long as they do not develop new symptoms.
- Unvaccinated people who have taken part in activities that put them at higher risk for COVID-19 because they cannot physically distance as needed to avoid exposure, such as travel, attending large social or mass gatherings, or being in crowded or poorly-ventilated indoor settings.
- People who have been asked or referred to get tested by their healthcare provider, or state, tribal, localexternal icon, or territorial health department.
CDC recommends that anyone with any signs or symptoms of COVID-19 get tested, regardless of vaccination status or prior infection. If you get tested because you have symptoms or were potentially exposed to the virus, you should stay away from others pending test results and follow the advice of your health care provider or a public health professional.
How to get tested for current COVID-19 infection
- Contact your healthcare provider or visit your state, tribal, local, and territorial health department’s website to find the latest local information on testing. The type of viral COVID-19 tests offered may differ by location.
You and your healthcare provider might also consider either an at-home collection kit or an at-home test if you have signs and symptoms of COVID-19 and if you can’t get tested by a healthcare provider or public health official.
How to use results of viral tests
- If you test positive, know what protective steps to take to prevent others from getting sick.
- If you test negative, you probably were not infected at the time your sample was collected. The test result only means that you did not have COVID-19 at the time of testing. Continue to take steps to protect yourself.
Quarantine and Isolation
You quarantine when you might have been exposed to the virus.
You isolate when you have been infected with the virus, even if you don’t have symptoms.
Quarantine
Quarantine if you have been in close contact (within 6 feet of someone for a cumulative total of 15 minutes or more over a 24-hour period) with someone who has COVID-19, unless you have been fully vaccinated. People who are fully vaccinated do NOT need to quarantine after contact with someone who had COVID-19 unless they have symptoms. However, fully vaccinated people should get tested 3-5 days after their exposure, even if they don’t have symptoms and wear a mask indoors in public for 14 days following exposure or until their test result is negative.
What to do
- Stay home for 14 days after your last contact with a person who has COVID-19.
- Watch for fever (100.4◦F), cough, shortness of breath, or other symptoms of COVID-19.
- If possible, stay away from people you live with, especially people who are at higher risk for getting very sick from COVID-19.
After quarantine
- Watch for symptoms until 14 days after exposure.
- If you have symptoms, immediately self-isolate and contact your local public health authority or healthcare provider.
You may be able to shorten your quarantine
Your local public health authorities make the final decisions about how long quarantine should last, based on local conditions and needs. Follow the recommendations of your local public health department if you need to quarantine. Options they will consider include stopping quarantine
- After day 10 without testing
- After day 7 after receiving a negative test result (test must occur on day 5 or later)
Isolation
Isolation is used to separate people infected with COVID-19 from those who are not infected.
People who are in isolation should stay home until it’s safe for them to be around others. At home, anyone sick or infected should separate from others, stay in a specific “sick room” or area, and use a separate bathroom (if available).
What to do
- Monitor your symptoms. If you have an emergency warning sign (including trouble breathing), seek emergency medical care immediately.
- Stay in a separate room from other household members, if possible.
- Use a separate bathroom, if possible.
- Avoid contact with other members of the household and pets.
- Don’t share personal household items, like cups, towels, and utensils.
- Wear a mask when around other people if able.
Learn more about what to do if you are sick and how to notify your contacts.
When You Can be Around Others After You Had or Likely Had COVID-19
Most people do not require testing to decide when they can be around others; however, if your healthcare provider recommends testing, they will let you know when you can resume being around others based on your test results.
For Anyone Who Has Been Around a Person with COVID-19
Anyone who has had close contact with someone with COVID-19 should stay home for 14 days after their last exposure to that person.
However, anyone who has had close contact with someone with COVID-19 and who meets the following criteria does NOT need to stay home.
- Someone who has been fully vaccinated and shows no symptoms of COVID-19. However, fully vaccinated people should get tested 3-5 days after their exposure, even they don’t have symptoms and wear a mask indoors in public for 14 days following exposure or until their test result is negative.
Or
- Someone who has COVID-19 illness within the previous 3 months and
- Has recovered and
- Remains without COVID-19 symptoms (for example, cough, shortness of breath)
When You’ve Been Fully Vaccinated- How to Protect Yourself and Others
If you’ve been fully vaccinated:
- You can resume activities that you did prior to the pandemic.
- To reduce the risk of being infected with the Delta variant and possibly spreading it to others, wear a mask indoors in public if you are in an area of substantial or high transmission.
- You might choose to wear a mask regardless of the level of transmission if you have a weakened immune system or if, because of your age or an underlying medical condition, you are at increased risk for severe disease, or if a member of your household has a weakened immune system, is at increased risk for severe disease, or is unvaccinated.
- You will still need to follow guidance at your workplace and local businesses.
- If you travel, you should still take steps to protect yourself and others.
- Wearing a mask over your nose and mouth is required on planes, buses, trains, and other forms of public transportation traveling into, within, or out of the United States and while indoors at U.S. transportation hubs such as airports and stations. Travelers are not required to wear a mask in outdoor areas of a conveyance (like on open deck areas of a ferry or the uncovered top deck of a bus).
- Fully vaccinated international travelers arriving in the United States are still required to get tested 3 days before travel by air into the United States (or show documentation of recovery from COVID-19 in the past 3 months) and should still get tested 3-5 days after their trip.
- You should still watch out for symptoms of COVID-19, especially if you’ve been around someone who is sick. If you have symptoms of COVID-19, you should get tested and stay home and away from others. If your test is positive, isolate at home for 10 days.
- People who have a condition or are taking medications that weaken the immune system, should continue to take all precautions recommended for unvaccinated people until advised otherwise by their healthcare provider.
Can Children Be Vaccinated Against COVID-19?
Is it safe for my child to get a COVID-19 vaccine/
Yes. Studies show that COVID-19 vaccines are safe and effective. Like adults, children may have some side effects after COVID-19 vaccination. These side effects may affect their ability to do daily activities, but they should go away in a few days. Children 12 years and older are now eligible to get vaccinated against COVID-19. COVID-19 vaccines have been used under the most intensive safety monitoring in U.S. history, including studies in children 12 years and older. Your child cannot get COVID-19 from any COVID-19 vaccine.
COVID-19 vaccination can help protect your child from getting COVID-19. Although fewer children have been sick with COVID-19 compared to adults, children can be infected with the virus that causes COVID-19, can get sick from COVID-19, and can spread the virus that causes COVID-19 to others. Getting your child vaccinated helps to protect your child and your family. Vaccination is now recommended for everyone 12 years and older. Currently, the Pfizer-BioNTech COVID-19 Vaccine is the only one available to children 12 years and older.
Information about COVID-19 Vaccines for Children and Teens
Cases of myocarditis and pericarditis in adolescents and young adults have been reported more often after getting the second dose than after the first dose of one of the two mRNA COVID-19 vaccines, Pfizer-BioNTech or Moderna. These reports are rare and the known and potential benefits of COVID-19 vaccination outweigh the known and potential risks, including the possible risk of myocarditis or pericarditis.
Get a COVID-19 vaccine for your child as soon as you can.
- COVID-19 vaccines are safe and effective.
- COVID-19 vaccines have been used under the most intensive safety monitoring in U.S. history, which includes studies in adolescents.
- Your child will need a second shot of the Pfizer-BioNTech COVID-19 Vaccine 3 weeks after their first shot.
- Children and adolescents receive the same dosage of Pfizer-BioNTech COVID-19 vaccine as adults. There are no patient weight requirements for COVID-19 vaccination, and COVID-19 vaccine dosage does not vary by patient weight.
- Your child can’t get COVID-19 from any COVID-19 vaccine, including the Pfizer-BioNTech vaccine.
- Your child may get a COVID-19 vaccine and other vaccines at the same visit or without waiting 14 days between vaccines.
Prepare for your child’s vaccination visit.
- Get tips for how to support your child before, during, and after the visit.
- Talk to your child before the visit about what to expect.
- Tell the doctor or nurse about any allergies your child may have.
- Comfort your child during the appointment.
- To prevent fainting and injuries related to fainting, your child should be seated or lying down during vaccination and for 15 minutes after the vaccine is given.
- After your child’s COVID-19 vaccination, you will be asked to stay for 15–30 minutes so your child can be observed in case they have a severe allergic reaction and need immediate treatment.
Possible side effects
Your child may have some side effects, which are normal signs that their body is building protection.

- Pain
- Redness
- Swelling
- Tiredness
- Headache
- Muscle pain
- Chills
- Fever
- Nausea
These side effects may affect your child’s ability to do daily activities, but they should go away in a few days. Some people have no side effects.
Ask your child’s healthcare provider for advice on using a non-aspirin pain reliever and other steps you can take at home to comfort your child. It is not recommended you give pain relievers before vaccination for the purpose of trying to prevent side effects.
COVID-19 Vaccine Booster Shot
When can I get a COVID-19 vaccine booster?
Not immediately. The goal is for people to start receiving a COVID-19 booster shot beginning in the fall, with individuals being eligible starting 8 months after they received their second dose of an mRNA vaccine (either Pfizer-BioNTech or Moderna). This is subject to authorization by the U.S. Food and Drug Administration and recommendation by CDC’s Advisory Committee on Immunization Practices (ACIP). FDA is conducting an independent evaluation to determine the safety and effectiveness of a booster dose of the mRNA vaccines. ACIP will decide whether to issue a booster dose recommendation based on a thorough review of the evidence.
Who will be the first people to get a booster dose?
If FDA authorizes and ACIP recommends a booster dose, the goal is for the first people eligible for a booster dose to be those who were the first to receive a COVID-19 vaccination (those who are most at risk). This includes healthcare providers, residents of long-term care facilities, and other older adults.
Why is the United States waiting to start offering COVID-19 vaccine boosters?
The COVID-19 vaccines authorized in the United States continue to be highly effective in reducing risk of severe disease, hospitalization, and death, even against the widely circulating Delta variant. However, COVID-19 constantly evolves. Experts are looking at all available data to understand how well the vaccines are working, including how new variants, like Delta, affect vaccine effectiveness. If FDA authorizes and ACIP recommends it, the goal is for people to start receiving a COVID-19 booster shot this fall.
Will people who received Johnson & Johnson’s Janssen (J&J/Janssen) COVID-19 Vaccine need a booster shot?
It is likely that people who received a J&J COVID-19 vaccine will need a booster dose. Because the J&J/Janssen vaccine wasn’t given in the United States until 70 days after the first mRNA vaccine doses (Pfizer-BioNTech and Moderna), the data needed to make this decision aren’t available yet. These data are expected in the coming weeks. With those data in hand, CDC will keep the public informed with a timely plan for J&J/Janssen booster shots.
Can people who received Johnson & Johnson’s Janssen (J&J/Janssen) COVID-19 Vaccine get a booster dose of an mRNA vaccine?
No, there aren’t enough data currently to support getting an mRNA vaccine dose (either Pfizer-BioNTech or Moderna) if someone has gotten a J&J/Janssen vaccine. People who got the J&J/Janssen vaccine will likely need a booster dose, and more data are expected in the coming weeks. With those data in hand, CDC will keep the public informed with a timely plan for J&J/Janssen booster shots.
If we need a booster dose, does that mean that the vaccines aren’t working?
No. COVID-19 vaccines are working very well to prevent severe illness, hospitalization, and death, even against the widely circulating Delta variant. However, with the Delta variant, public health experts are starting to see reduced protection against mild and moderate disease. For that reason, the U.S. Department of Health and Human Services (HHS) is planning for a booster shot so vaccinated people maintain protection over the coming months.
What’s the difference between a booster dose and an additional dose?
Sometimes people who are moderately to severely immunocompromised do not build enough (or any) protection when they first get a vaccination. When this happens, getting another dose of the vaccine can sometimes help them build more protection against the disease. This appears to be the case for some immunocompromised people and COVID-19 vaccines. CDC recommends moderately to severely immunocompromised people consider receiving an additional (third) dose of an mRNA COVID-19 vaccine (Pfizer-BioNTech or Moderna) at least 28 days after the completion of the initial 2-dose mRNA COVID-19 vaccine series.
In contrast, a “booster dose” refers to another dose of a vaccine that is given to someone who built enough protection after vaccination, but then that protection decreased over time (this is called waning immunity). HHS has developed a plan to begin offering COVID-19 booster shots to people this fall. Implementation of the plan is subject to FDA’s authorization and ACIP’s recommendation.
Myths and Facts about COVID-19 Vaccines
How do I know which COVID-19 vaccine information sources are accurate?
Accurate vaccine information is critical and can help stop common myths and rumors.
It can be difficult to know which sources of information you can trust. Before considering vaccine information on the Internet, check that the information comes from a credible source and is updated on a regular basis.
Errands and Going Out- Staying Safe and Healthy
As communities and businesses continue to reopen, US CDC has provided guidance on resuming daily activities such as errands as safely as possible.
US CDC states that while there is no way to ensure zero risk, it is important to understand potential risks and how to adopt different types of prevention measures to protect yourself and to help reduce the spread of COVID-19.
In general, the more closely you interact with others and the longer that interaction, the higher the risk of COVID-19 spread.
So, think about:
- How many people will you interact with?
- Interacting with more people raises your risk.
- Being in a group with people who aren’t social distancing or wearing cloth face coverings increases your risk.
- Engaging with new people (e.g., those who don’t live with you) also raises your risk.
- Some people have the virus and don’t have any symptoms, and it is not yet known how often people without symptoms can transmit the virus to others.
- Can you keep 6 feet of space between you and others? Will you be outdoors or indoors?
- The closer you are to other people who may be infected, the greater your risk of getting sick.
- Keeping distance from other people is especially important for people who are at higher risk for severe illness, such as older adults and those with underlying medical conditions.
- Indoor spaces are more risky than outdoor spaces where it might be harder to keep people apart and there’s less ventilation.
- What’s the length of time that you will be interacting with people?
- Spending more time with people who may be infected increases your risk of becoming infected.
- Spending more time with people increases their risk of becoming infected if there is any chance that you may already be infected.
Please visit US CDC's website for detailed information on this topic.
NEW: Check out this helpful document created by our team to assist you in keeping your outings "Safe and healthy"
If You are Sick
If you have confirmed or suspected COVID-19, follow these steps from US CDC:
Download the Managing Respiratory Symptoms at Home fact sheet.
- Stay home from work, school, and away from other public places. If you must go out, avoid using any kind of public transportation, ridesharing, or taxis.
- Monitor your symptoms carefully. If your symptoms get worse, call your healthcare provider immediately.
- Get rest and stay hydrated.
- If you have a medical appointment, call the healthcare provider ahead of time and tell them that you have or may have COVID-19.
- For medical emergencies, call 911 and notify the dispatch personnel that you have or may have COVID-19.
- Cover your cough and sneezes.
- Wash your hands often with soap and water for at least 20 seconds or clean your hands with an alcohol-based hand sanitizer that contains at least 60% alcohol.
- As much as possible, stay in a specific room and away from other people in your home. Also, you should use a separate bathroom, if available. If you need to be around other people in or outside of the home, wear a facemask.
- Avoid sharing personal items with other people in your household, like dishes, towels, and bedding
- Clean all surfaces that are touched often, like counters, tabletops, and doorknobs. Use household cleaning sprays or wipes according to the label instructions.
When to Seek Medical Attention
If you develop emergency warning signs for COVID-19 get medical attention immediately. Emergency warning signs include*:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
*This list is not all inclusive. Please consult your medical provider for any other symptoms that are severe or concerning.
Hand Washing Info
Hand washing is one of the most important ways you can keep from getting sick and spreading germs to others. It is a simple but mighty tool! Soap destroys the virus, but we need to wash our hands for twenty seconds for it to work.
Follow these directions for hand washing.
- Wash your hands often with soap and water for at least 20 seconds especially after you have been in a public place, or after blowing your nose, coughing, or sneezing. Click here to watch a quick video on proper hand washing.
- If soap and water are not available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Additional key times to clean hands include:
After using the restroom
Before eating or preparing food
After contact with animals or pets
Before and after providing routine care for another person who needs assistance (e.g. a child)
Household Cleaning and Disinfecting Directions
If someone in your home is sick, disinfecting and safely dealing with dishes, laundry, and trash will help protect others. Follow the US CDC directions to disinfect your home. Download the Everyday Cleaning and Disinfecting handout.
US CDC recommends daily cleaning and disinfecting of regularly touched areas like: tables, doorknobs, light switches, counter tops, handles, desks, phones, keyboards, toilets, faucets, sinks, etc.
The first step is to clean surfaces if they are dirty. Use detergent or soap and water for this part of the job.
Next, it's time to disinfect.
To disinfect:
Most common EPA-registered household disinfectants will work. Use disinfectants appropriate for the surface.
Options include:
- Diluting your household bleach.
To make a bleach solution, mix:- 5 tablespoons (1/3rd cup) bleach per gallon of water
OR - 4 teaspoons bleach per quart of water. Follow manufacturer’s instructions on how to apply and how much fresh air (ventilation) is needed. Check to ensure the bleach is not past its expiration date. Never mix household bleach with ammonia or any other cleanser.
- 5 tablespoons (1/3rd cup) bleach per gallon of water
- Alcohol solutions.
Make sure the solution has at least 70% alcohol. - Other common EPA-registered household disinfectants.
Products with EPA-approved emerging viral pathogens claims are expected to be effective against COVID-19 based on data for harder to kill viruses. Follow the manufacturer’s instructions for all cleaning and disinfection products (e.g., concentration, application method and contact time, etc.).
Click here for detailed disinfecting directions.
What We Know About the Omicron Variant
https://www.cdc.gov/coronavirus/2019-ncov/variants/omicron-variant.html
Omicron Variant: What You Need to Know
Omicron in the United States
CDC is working with state and local public health officials to monitor the spread of Omicron. As of December 20, 2021, Omicron has been detected in most states and territories and is rapidly increasing the proportion of COVID-19 cases it is causing.
CDC is expecting a surge of COVID-19 cases in the coming days to weeks. Learn more about Omicron variant surveillance and potential rapid spread.
What We Know about Omicron
CDC has been collaborating with global public health and industry partners to learn about Omicron, as we continue to monitor its course. We don’t yet know how easily it spreads, the severity of illness it causes, or how well available vaccines and medications work against it.
Spread
The Omicron variant likely will spread more easily than the original SARS-CoV-2 virus and how easily Omicron spreads compared to Delta remains unknown. CDC expects that anyone with Omicron infection can spread the virus to others, even if they are vaccinated or don’t have symptoms.
Severe Illness
More data are needed to know if Omicron infections, and especially reinfections and breakthrough infections in people who are fully vaccinated, cause more severe illness or death than infection with other variants.
Vaccines
Current vaccines are expected to protect against severe illness, hospitalizations, and deaths due to infection with the Omicron variant. However, breakthrough infections in people who are fully vaccinated are likely to occur. With other variants, like Delta, vaccines have remained effective at preventing severe illness, hospitalizations, and death. The recent emergence of Omicron further emphasizes the importance of vaccination and boosters.
Treatments
Scientists are working to determine how well existing treatments for COVID-19 work. Based on the changed genetic make-up of Omicron, some treatments are likely to remain effective while others may be less effective.
We have the Tools to Fight Omicron
Vaccines
Vaccines remain the best public health measure to protect people from COVID-19, slow transmission, and reduce the likelihood of new variants emerging.
- COVID-19 vaccines are highly effective at preventing severe illness, hospitalizations, and death.
- Scientists are currently investigating Omicron, including how protected fully vaccinated people will be against infection, hospitalization, and death.
- CDC recommends that everyone 5 years and older protect themselves from COVID-19 by getting fully vaccinated.
- CDC recommends that everyone ages 16 years and older get a booster shot after completing their primary COVID-19 vaccination series. You are eligible for a booster at 5 months after completing Pfizer-BioNTech primary series, 6 months after completing Moderna primary series, and 2 months after the initial J&J/Janssen vaccine. Individuals ages 16-17 are only eligible for the Pfizer-BioNTech COVID-19 vaccine.
Masks
Masks offer protection against all variants.
- CDC continues to recommend wearing a mask in public indoor settings in areas of substantial or high community transmission, regardless of vaccination status.
- CDC provides advice about masks for people who want to learn more about what type of mask is right for them depending on their circumstances.
Testing
Tests can tell you if you are currently infected with COVID-19.
- Two types of tests are used to test for current infection: nucleic acid amplification tests (NAATs) and antigen tests. NAAT and antigen tests can only tell you if you have a current infection.
- Individuals can use the COVID-19 Viral Testing Tool to help determine what kind of test to seek.
- Additional tests would be needed to determine if your infection was caused by Omicron.
- Visit your state, tribal, local, or territorial health department’s website to look for the latest local information on testing.
- Self-tests can be used at home or anywhere, are easy to use, and produce rapid results.
- If your self-test has a positive result, stay home or isolate for 10 days, wear a mask if you have contact with others, and call your healthcare provider.
- If you have any questions about your self-test result, call your healthcare provider or public health department.
Until we know more about the risk of Omicron, it is important to use all tools available to protect yourself and others.
What CDC is Doing to Learn about Omicron
Virus Characteristics
CDC scientists are working with partners to gather data and virus samples that can be studied to answer important questions about the Omicron variant. Scientific experiments have already started. CDC will provide updates as soon as possible.
Variant Surveillance
In the United States, CDC uses genomic surveillance to track variants of SARS-CoV-2, the virus that causes COVID-19 to more quickly identify and act upon these findings to best protect the public’s health. CDC established multiple ways to connect and share genomic sequence data being produced by CDC, public health laboratories, and commercial diagnostic laboratories within publicly accessible databases maintained by the National Center for Biotechnology Informationexternal icon (NCBI) and the Global Initiative on Sharing Avian Influenza Dataexternal icon (GISAID). If a variant is circulating at 0.1% frequency, there is a >99% chance that it will be detected in CDC’s national genomic surveillance.
On November 24, 2021, South Africa reported the identification of a new SARS-CoV-2 variant, B.1.1.529, to the World Health Organization (WHO). B.1.1.529 was first detected in specimens collected on November 11, 2021 in Botswana and on November 14, 2021 in South Africa.
Emergence of Omicron
CDC has been using genomic surveillance throughout the course of the pandemic to track variants of SARS-CoV-2, the virus that causes COVID-19, and inform public health practice.
- November 24, 2021: A new variant of SARS-CoV-2, B.1.1.529, was reported to the World Health Organization (WHO). This new variant was first detected in specimens collected on November 11, 2021 in Botswana and on November 14, 2021 in South Africa.
- November 26, 2021: WHO named the B.1.1.529 Omicron and classified it as a Variant of Concern (VOC).
- November 30, 2021: The United States designated Omicron as a Variant of Concern.
- December 1, 2021: The first confirmed U.S. case of Omicron was identified.
: